Abstract
Philadelphia chromosome-like acute lymphoblastic leukemia (Ph-like ALL) represents 20% of newly diagnosed adults with B cell ALL (B-ALL), with increased frequency in adults with Hispanic ethnicity. Ph-like ALL harbors a diverse range of genetic alterations with CRLF2-rearrangement/overexpression (CRLF2r) being the most common one. When treated with chemotherapy, Ph-like ALL is associated with inferior response, high relapse rate, and low overall survival (OS). Allogenic hematopoietic cell transplantation (alloHCT) is a well-established curative modality for adults with high-risk ALL. Considering that Ph-like ALL is a high-risk leukemia subtype, it is appealing to recommend alloHCT consolidation routinely for this entity in adults. However, large datasets describing alloHCT outcomes in patients with Ph-like ALL is lacking.
In this study, we retrospectively analyzed archived DNA samples from 125 consecutive adult patients with Ph-negative ALL who underwent alloHCT in complete remission (CR) at our center between 2006 and 2020. Classification of Ph-like versus non-Ph-like was performed according to WHO 2017 classification using accumulative results from RNAseq, conventional cytogenetics, FISH, and whole genome array studies. A proprietary RNA sequencing assay covering 1,188 genomic regions from 235 genes was designed to detect all the clinically significant fusions and expressions for Ph-like ALLs. In addition, an algorithm employing the RNAseq data was developed to further aid in classification of Ph-like ALL.
Boruta feature selection (R package "Boruta" version 7.0.0) was used to identify the most informative genes for prediction with an out-of-bag error of 9.62%. The following 24 genes were identified: CCND2, SOX11, PAX5, DENND3, RARA, MME, ID4, SH3BP5, HOXA9, CA6, MUC4, CYB5R2, CD97, EPOR, IL2RA, RAB29, PDGFRA, MLLT4, RHOA, JAK2, DNM2, ASXL1, BCL2A1, and KDR. The results were used to predict Ph-like status by a Random Forest model (R package "randomForest" version 4.6-14) that generates a probability/similarity score of Ph gene expression profile (Ph score). The testing samples with Ph score over 50% and without other subtype-defining lesions are defined as Ph-like.
We identified Ph-like genetic alterations in 66 (53%) patients, of whom 42 (66%) were carrying CRLF2r and 24 (36%) were non-CRLF2r. Compared to non-Ph-like ALL (n=59), Ph-like ALL patients were younger (42 vs 36 years old, p=0.022), more frequently Hispanic (56% vs 83%, p=0.003), less frequently carried high-risk cytogenetics (39% vs 9%, p<0.001), more frequently induced with pediatric-inspired regimens (25% vs 61%, p=0.003) and more likely required >1 regimen to achieve their first complete remission (CR1; 30% vs 55%, p=0.025). However, we did not detect any significant difference between the two groups in disease status (CR1 vs. CD2/3; p=0.81) or minimal residual disease clearance at the time of HCT (negative vs. positive; p=0.17), donor type (match related/unrelated vs mismatch vs haplo vs cord blood; p=0.88), conditioning regimen intensity (myeloablative vs non-myeloablative/ reduced intensity; p=0.59), GVHD prophylaxis (tacrolimus/sirolimus-based vs PTCy-based; p=0.84), Karnofsky Performance Status (KPS; p=0.24) or HCT comorbidity index (0 vs 1-2 vs >2; p=0.42).
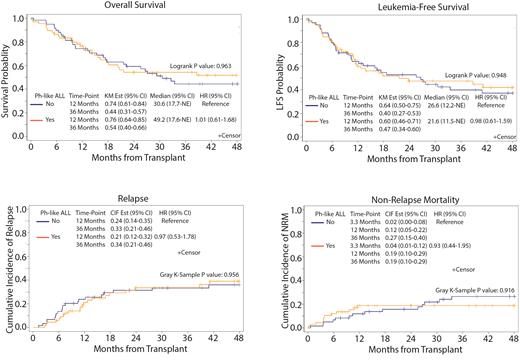
With the median follow-up of 3.2 years, we observed similar 3-years leukemia-free survival (LFS) (40% vs 47%; p=0.95), OS (44% vs 54%; p=0.96), relapse rate (33% vs 34%; p=0.96) and non-relapse mortality (NRM) (27% vs 19%; p=0.92) between non-Ph-like and Ph-like ALL patients, respectively. (Figure) In multivariable analysis, disease status at the time of HCT (HR=2.63, 95% CI: 1.57-4.41; p<0.001), donor type (p=0.049) and KPS (HR=2.22, 95% CI: 1.05-4.69; p=0.038) influenced OS. LFS was significantly influenced by disease status (HR=2.35, 95% CI: 1.45-3.80); p<0.001) and conditioning regimen intensity (HR=1.84, 95% CI: 1.11-3.04; p=0.017). Relapse rate was associated with disease status (HR=2.06, 95%CI: 1.11-3.84; p=0.23) and conditioning regimen intensity (HR=1.97, 95% CI: 1.03-3.75; p=0.40). Only KPS (HR=6.56, 95% CI: 2.48-17.36; P<0.001) was associated with NRM.
In conclusion, our data suggest that alloHCT consolidation results in favorable outcomes in adult patients with Ph-like ALL with comparable outcomes to non-Ph-like ALL. Our data support utilization of alloHCT for adults with Ph-like ALL in CR.
Al Malki: Neximmune: Consultancy; Rigel Pharma: Consultancy; Jazz Pharmaceuticals, Inc.: Consultancy; Hansa Biopharma: Consultancy; CareDx: Consultancy. Khaled: Omeros: Honoraria; Alexion: Honoraria, Speakers Bureau; Janssen: Current Employment; Astellas: Honoraria; Jazz: Honoraria. Ali: Incyte: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; BMS: Speakers Bureau; CTI BioPharma: Membership on an entity's Board of Directors or advisory committees. Aribi: Seagen: Consultancy. Mei: BMS: Research Funding; Epizyme: Research Funding; TG Therapeutics: Research Funding; EUSA: Honoraria; Janssen: Honoraria; Morphosys: Research Funding; Beigene: Research Funding. Koller: Novartis: Consultancy. Artz: Radiology Partners: Other: Spouse has equity interest in Radiology Partners, a private radiology physician practice. Stein: Amgen: Consultancy, Speakers Bureau; Celgene: Speakers Bureau; Stemline: Speakers Bureau. Marcucci: Abbvie: Other: Speaker and advisory scientific board meetings; Novartis: Other: Speaker and advisory scientific board meetings; Agios: Other: Speaker and advisory scientific board meetings. Forman: Lixte Biotechnology: Consultancy, Current holder of individual stocks in a privately-held company; Mustang Bio: Consultancy, Current holder of individual stocks in a privately-held company; Allogene: Consultancy. Pullarkat: AbbVie, Amgen, Genentech, Jazz Pharmaceuticals, Novartis, Pfizer, and Servier: Membership on an entity's Board of Directors or advisory committees; Amgen, Dova, and Novartis: Consultancy, Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal